The story of modern healthcare has a paradox: the very system designed to save clinicians time often takes it away.
Electronic Health Records (EHRs), the digital platforms that store everything from lab results to clinical notes, were designed to replace the endless paper charts. They became the backbone of the hospitals around the world. And yet today, doctors spend up to half their workday inside the EHR, clicking through fragmented screens while patients wait.
AI in EHR entered the scene like a plot twist.
Now, EHR systems can listen and write notes as the physician speaks, which enables predictions of complications days before symptoms appear, and translates scattered data into a single, clear picture of the patient.
This isn’t science fiction; it’s already happening in several hospitals worldwide. But the burning question is — will healthcare leaders take advantage of AI to reduce burnout, cut costs, and improve outcomes? Or will they simply watch the next wave of transformation pass them by?
What are the challenges with the traditional EHR systems?

Electronic Health Records are now used in almost every hospital and clinic, but they still present significant challenges. These issues impact the speed at which doctors can work, the safety of patient care, and the overall efficiency of hospitals.
Here are four major challenges that stand out:
Data fragmentation and interoperability issues
Many EHR systems keep patient information locked in separate databases, which makes it hard for doctors to see a complete record in one place.
Even after years of government efforts, only about 70% of U.S. hospitals share patient data across all main areas of care, and fewer than half do it regularly. Smaller and rural hospitals struggle even more.
This means doctors often don’t have quick access to lab results, medical history, or test reports from outside facilities. Without proper data sharing, care gets delayed, and tests are often repeated unnecessarily. As one study noted,
“The fragmentation of health data across disparate EHR systems has hindered the realization of their full potential.”
Clinician burnout due to documentation burden
Instead of saving time, EHRs often increase the amount of paperwork doctors must complete. Physicians spend 34 to 55% of their workday filling out EHR forms, answering inbox messages, and managing orders. This takes valuable time away from patients and forces clinicians into clerical work they did not expect when entering medicine.
Studies also link heavy EHR use to higher burnout and lower job satisfaction. Doctors often end up charting late into the evening, which can lead to frustration, stress, and sometimes early exits from the profession.
Inaccurate or delayed clinical decision-making
EHRs were supposed to help doctors make better decisions, but how often do they deliver?
Complex EHR systems often make it difficult for clinicians to locate the right information quickly. Interfaces are often cluttered with a large number of alerts, which can cause fatigue and make it easier to overlook important warnings.
Delays in retrieving patient histories or lab results can postpone care, while excessive or irrelevant alerts can cause doctors to dismiss notifications altogether. In both cases, the outcome is slower and less reliable decision-making.
Compliance and regulatory challenges
EHR systems must also meet strict privacy and regulatory requirements. For example, HIPAA sets clear limits on how patient information can be stored, accessed, and shared. Using health data for advanced purposes, such as training AI systems, often requires additional safeguards and, in many cases, patient authorization.
Hospitals also rely on EHRs to meet mandatory reporting requirements and support audits and investigations. While these regulations protect patients, they add technical complexity to system design and increase the administrative workload for healthcare staff.
Together, these challenges highlight the limits of traditional EHRs and set the stage for AI-driven solutions. AI in EHR can address inefficiencies, reduce stress on clinicians, and improve patient outcomes.
Let’s see how.
How can AI enhance EHR functionality?
Artificial intelligence (AI) is changing how EHR systems operate at a fundamental level. Instead of simply storing and organizing patient information, AI-enabled software can automate, predict, and support clinical decisions in ways that ease clinician workloads and improve care quality.
Here are four major enhancements AI offers to EHR:
Can AI automate data entry and transcription?
One of the most immediate benefits of generative AI is in documentation. Using natural language processing (NLP), AI-powered ambient scribes can listen to a physician-patient conversation and automatically generate structured notes inside the EHR. These tools can:
- Speed up documentation
- Reduce administrative burden
- Allow providers to pay more attention to the patients
By converting speech into accurate, structured records, AI eliminates one of the primary pain points of modern EHR use: the need for endless typing. But even partial automation, such as extracting key details from free-text notes and filling in standard fields, saves time and lowers human errors.
How can predictive analytics improve patient care?
AI can also make EHRs proactive rather than reactive. Predictive algorithms analyze data from labs, vital signs, notes, and demographics to identify patients who are likely to develop complications.
About 65% of U.S. hospitals already use predictive models integrated into their EHRs. Most commonly, they are applied to track inpatient trajectories or to identify high-risk outpatients who need follow-up.
Unlike traditional rule-based alerts, machine learning (ML) can identify subtle signals, such as slight shifts in vital signs. Combined with lab results, these alerts can flag patients for targeted preventive care for conditions that are likely to deteriorate, such as sepsis and heart conditions.
As a result, healthcare organizations can prioritize earlier intervention, fewer missed diagnoses, and better allocation of clinical resources.
What role does AI play in clinical decision support?
Decision support has always been an integral part of EHRs, typically in the form of alerts about drug interactions, allergy warnings, or reminders to order screenings. AI takes this capability much further by utilizing ML-based CDSS and training on large datasets to provide personalized recommendations for individual patients, rather than generic alerts.
Hospitals are beginning to use AI-driven CDSS to predict deterioration, improve adherence to clinical guidelines, and prioritize alerts more intelligently (AHRQ). This helps reduce “alert fatigue” while improving accuracy.
However, experts do stress that these systems must be transparent and rigorously validated so that clinicians trust the recommendations. Therefore, an AI-powered CDSS must be built to act like a real partner in care rather than just another pop-up in the workflow. It must be designed well by experts who understand data-transparency requirements and compliance in the medical system.
Can AI improve data mapping and interoperability?
One of the most important, yet less obvious, uses of AI is in facilitating communication between different healthcare systems.
Many hospitals use different formats for storing records, which makes it hard to share information quickly. AI tools, including advanced large language models (LLMs), can read doctors’ notes and automatically convert them into standard formats that every system can understand.
In one study, AI achieved nearly 88% accuracy in converting free-text notes, such as “chest pain,” into official diagnostic codes. In practice, this means:
- Hospitals spend less time cleaning up data
- Doctors receive a more comprehensive view of the patient’s history
- There’s less delay in exchanging information between systems
AI won’t solve every data-sharing problem, but it makes the process faster and more reliable than before.
Benefits of AI integration in EHRs
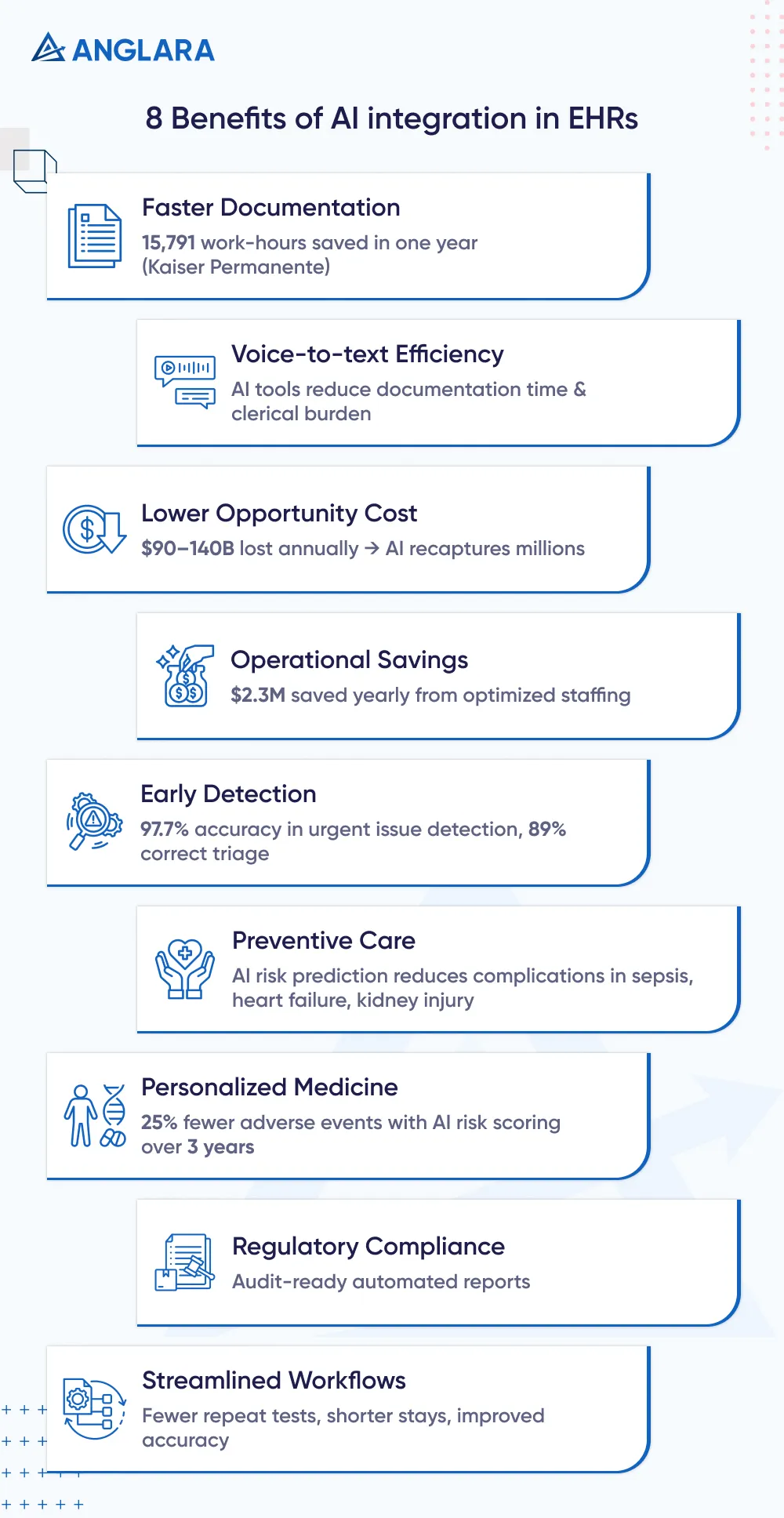
Hospitals and clinics that integrate AI into their EHR systems report improvements across multiple fronts, from time savings to better patient safety to improved financial performance. Here are some clear benefits of AI integration in EHRs:
- Faster documentation: Kaiser Permanente physicians using AI scribes saved 15,791 work-hours in one year, freeing significant clinical capacity.
- Voice-to-text efficiency: Research shows that nearly all AI voice-to-text systems reduce documentation time and clerical burden.
- Lower opportunity cost: U.S. physicians lose an estimated $90 to $140 billion annually on charting. Even modest AI-driven reductions recapture millions of dollars in value.
- Operational savings: Predictive AI has been utilized to optimize staffing, resulting in a $2.3 million annual savings for one health system by reducing reliance on temporary staff during peak demand.
- Early detection with fewer errors: AI-enabled patient portals at Kaiser flagged urgent issues with 97.7% accuracy and guided patients to the right care in nearly 89% of cases.
- Preventive care: Algorithms that predict risks, such as sepsis, heart failure, and acute kidney injury, can enable earlier treatment and fewer complications.
- Personalized medicine: AI uses genomic data and risk scores to tailor care. In one case, applying polygenic risk scores for heart disease and providing proactive coaching to high-risk patients resulted in a 25% reduction in adverse events over a three-year period.
- Regulatory compliance: Automated tools generate complete, audit-ready records that meet accreditation standards such as JCAHO.
- Streamlined workflows: Fewer repeated tests, shorter lengths of stay, and improved documentation accuracy all contribute to measurable financial savings.
Considerations of AI implementation in EHR
AI offers clear advantages, but bringing it into the complex world of healthcare requires careful planning. Here are common challenges of implementing AI in medical settings:
How can hospitals ensure data privacy and HIPAA compliance with AI?
Any AI system that processes protected health information (PHI) is subject to HIPAA rules. This means data use must meet the “minimum necessary” standard, and in some cases, requires the patient’s explicit authorization.
Large-scale AI training can be difficult under these restrictions. The fact that many AI vendors rely on cloud services adds another layer of risk, as hospitals must also ensure compliance across third-party platforms.
The solution: Hospitals should adopt rigorous governance frameworks for the use of AI data, including:
- Clear policies on what PHI can be shared
- Encryption of all data transfers
- Rigorous vendor vetting
- Regular audits and HIPAA risk assessments
Using de-identified or synthetic data for model training can help reduce compliance burdens while still supporting innovation.
How can AI integrate with legacy EHR systems?
Most U.S. hospitals still run on large, complex EHRs that were not originally designed for AI, like Epic or Cerner EHR (now Oracle).
Connecting AI tools to these systems often requires custom integration work, middleware, or API development to facilitate seamless communication. Only 46% of post-acute care providers report having easy data exchange with outside partners, which highlights the continued fragmentation of the ecosystem. These technical barriers can slow adoption and increase upfront costs.
The solution: Hospitals should start with pilot projects in targeted areas. For example, ambient scribes within a single department or predictive analytics for a specific patient population. Utilizing standards like FHIR APIs can reduce the need for custom integrations over time.
Partnering with vendors that have proven interoperability capabilities is also key. In the long term, organizations need an IT roadmap that modernizes infrastructure in phases, rather than attempting a full overhaul at once.
How can transparency, explainability, and bias be addressed in AI models?
Many AI models operate like “black boxes,” producing outputs without clear reasoning, making clinicians hesitant to rely on them. Worse, without local testing, algorithms may reflect biases that disadvantage certain patient groups.
Alarmingly, 56% of hospitals using predictive models had never checked them for bias. And when left unchecked, this can widen health disparities instead of reducing them.
The solution: Every AI tool integrated must have an explainability feature that shows why a recommendation was made, for example, key factors driving a risk score. Hospitals must:
- Perform local validation before deployment
- Ensure the model performs well across their own patient population
- Build in ongoing monitoring for bias into governance processes
- Set a clear path for clinicians to override AI outputs when necessary
Several regulatory bodies require EHR vendors to disclose model validation and bias-mitigation methods in their certification filings, providing hospitals with more transparency to work with.
What training and adoption support do clinicians need for AI?
Even the most advanced AI tool has little impact if clinicians pick it up promptly. And let us tell you, adoption is uneven. While 66% of U.S. physicians now use some form of health AI, only 20% of staff in many organizations have received structured training.
Some clinicians remain skeptical of AI or resist changes that disrupt workflows.
The solution: Hospitals need a structured change-management plan, which includes:
- Training programs tailored to different roles
- Hands-on demonstrations
- Ongoing technical support
Clinician involvement in the early design and feedback process makes tools more user-friendly and increases trust. Above all, the focus should be on demonstrating how AI reduces workload and supports improved patient care, rather than presenting it as just another IT system to learn.
Addressing these challenges upfront ensures that AI can be deployed responsibly and sustainably, and choosing the right partner for implementation becomes crucial. Collaborate with AI consulting experts to assess use cases, develop a phased adoption roadmap, and optimize ROI while mitigating common pitfalls. They can guide hospitals through complex integrations, ensure compliance, and tailor AI solutions to local needs.
So are the benefits worth the cost of AI implementation?
Bringing AI into EHR systems does require a considerable investment, but are the returns worth it? Short answer — absolutely. But don’t just take what we say, understand the “why” behind it.
Hospitals need to account for two categories of spending:
- Initial setup: Software licensing, infrastructure upgrades, and staff training.
- Ongoing operations: Subscription fees, updates, maintenance, and compliance safeguards.
Costs also vary depending on system complexity — a large, multi-site hospital may pay more than a smaller community clinic due to integration and customization needs.
However, the key point is that while the investment is real, the payoff is even more significant.
At Kaiser Permanente, physicians using AI scribes freed up the time equivalent of eight full-time providers. Another Kaiser initiative enhanced patient engagement by increasing appointment-booking success from 30% to over 50%, reducing appointment no-shows from 30% to just 3%, and improving patient satisfaction scores.
Our predictive AI scheduling and smart triage helped clinics juggle no-shows, overbooked slots, and uneven staff loads. It forecasts appointment demand, predicting no-show risk, and recommending slot rebalancing.
What Anglara delivered:
- Smoother Schedules: Fewer last-minute gaps and better clinician utilization.
- Faster First Contact: Patients routed correctly without repeat booking.
- Lower Admin Load: Fewer calls and manual reschedules for staff.
- Higher Satisfaction: Clear instructions and reminders reduce confusion.
Read more about Predictive AI Scheduling and Smart Triage for Clinics.
Results like these translate directly into better resource use, higher reimbursement, and improved care quality.
Major health systems like Mayo Clinic, Epic, and Cerner are all actively building AI into their platforms because they recognize the ROI potential. For smaller and mid-sized providers, the question is not whether AI will deliver returns, but how to implement it effectively.
That’s where having the right partner makes a difference. At Anglara, we help healthcare organizations design AI strategies that strike a balance between upfront costs and measurable outcomes. From pilot programs to full-scale rollouts. Our focus is on aligning AI with real clinical and financial goals.
Check out our case studies to see how we deliver on our promise. Schedule a free consultation with our experts to explore how Anglara can help you integrate AI seamlessly across the organization.