Healthcare administrative costs consume $166 billion annually across U.S. hospitals — that’s a whopping 17% of total expenses. Prior authorization delays from insurers affect 94% of physicians, and 24% report serious adverse patient events as a result. Plus, hospitals spend $10-20 billion annually just to meet insurer requirements.
Now, with AI agents in the picture, the reality can be different.
AI agent use cases in healthcare include automating repetitive workflows, reducing approval times from 8-10 days to 24-48 hours, and freeing clinical teams to focus on patient care rather than paperwork.
But deploying AI agents in healthcare isn't like deploying them in other industries. Patient safety, HIPAA compliance, and clinical oversight must come first.
Read along to the end and learn how to implement AI agents for your institution, keeping compliance in mind for use cases that deliver solid ROI.
What are the top administrative AI agent use cases for healthcare?
AI in Healthcare can be a transformative force, improving patient care and diagnosis. However, one of the most important uses of AI is deploying agents to automate redundant tasks that consume a lot of your medical team’s time. These administrative tasks prevent them from giving their patients the utmost attention.
With AI agents at work, your doctors, nurses, and other clinical staff can focus purely on making the patient experience delightful. Here are the top administrative use cases of AI agents in healthcare:
Prior authorization preparation & submission
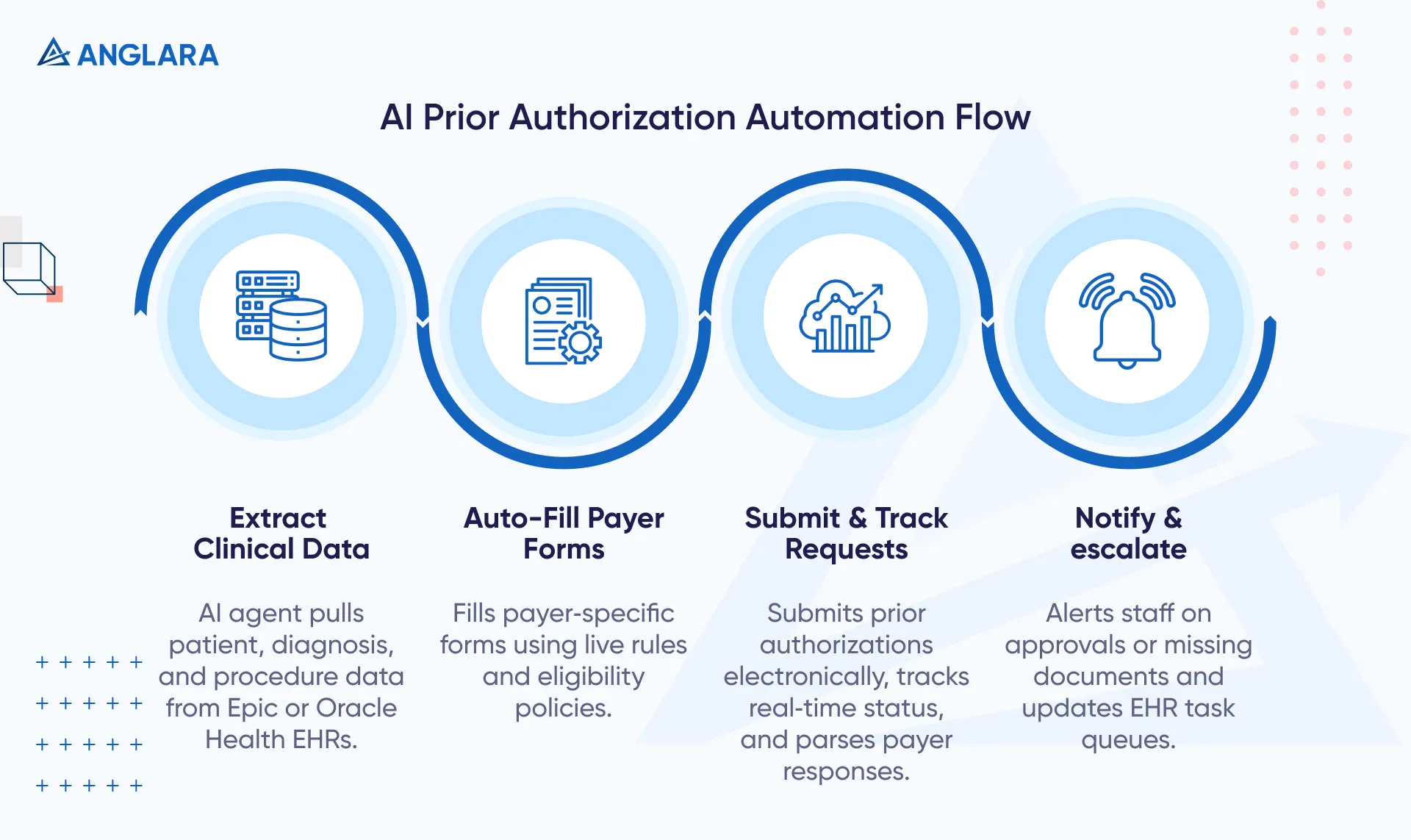
Prior authorization consumes 12+ hours of staff time per physician per week. Manual processes involve endless faxes, phone calls, and payer-specific forms that are constantly changing. AI agents can automate the entire workflow:
- Extract relevant clinical data from EHR systems like Epic or Oracle
- Fill payer-specific forms automatically based on real-time rules
- Submit requests electronically and track status updates
- Alert staff when approvals arrive or additional documentation is needed
Organizations using AI-powered prior authorization see dramatic results. Humana, an American health insurance company, implemented an AI platform across 12 states for musculoskeletal services, and achieved:
- 89% immediate approvals with a median approval time of 0 minutes.
- Automated processing of 95% of all MSK authorization requests digitally.
- Provider satisfaction with the “very satisfied” rate booted to 72%.
- Provider Net Promoter Scores increased by more than 100%.
In another case, a Blue Plan client achieved:
- 93% digital adoption shortly after launch
- Daily provider call reduction by one-third and a significant cut in fax-based communications
KPIs to track: Approval turnaround time, denial rates avoided, staff hours saved per authorization, and first-pass approval rate.
Revenue cycle (eligibility, coding assist, claim status)
Revenue cycle management involves checking patient eligibility, coding procedures correctly, submitting claims, and following up on payment status. The medical codes involved typically include:
- International Classification of Diseases (ICD) codes for diagnoses
- Current Procedural Terminology (CPT) codes for procedures
- Healthcare Common Procedure Coding System (HCPCS) codes for supplies and services
- Diagnosis-Related Group (DRG) codes for inpatient cases
Accurate coding is essential for compliant and timely billing. Manual handling of these tasks creates bottlenecks, errors, and delayed reimbursement. AI agents can streamline this entire cycle by:
- Verifying insurance eligibility in real-time before appointments
- Drafting accurate medical codes for clinician review, reducing errors by 70%
- Submitting clean claims automatically, improving first-pass acceptance
- Tracking claim status proactively and following up on denials
ApolloMD is an American physician-owned group practice that provides multi-specialty physician services, such as emergency medicine, hospital medicine, anesthesia, and radiology, to over 100 healthcare institutions. It implemented AI agents to optimize revenue cycle workflows, achieving 90% autonomous issue resolution and saving thousands of staff hours.
Many organizations report 30% faster claim processing times and a 4.6% monthly reduction in denials. Providers can achieve up to 10x ROI by automating these workflows, reducing labor costs, and accelerating cash flow.
KPIs to track: First-pass claim yield, days in accounts receivable, clean claim rate, and denial reduction percentage.
Patient access & scheduling
Traditional phone-based scheduling frustrates patients and overwhelms staff. Patients face long hold times, and 60% won't wait more than one minute.
Staff spend 5-6 hours daily just on confirmations and cancellations, but things change drastically when you let AI agents handle patient access workflows. Here’s what AI agents do:
- Conduct conversational intake via voice or chat to understand patient needs
- Capture insurance information and verify eligibility automatically
- Book appointments based on provider availability and patient preferences
- Send automated reminders via SMS, email, or calls to reduce no-shows
Real-world results are striking. Emirates Health Services reduced no-show rates from 21% to 10% in the USA. That’s a 57% drop, all through AI scheduling. Mayo Clinic, on the other hand, used AI agents, reducing doctors' time spent on electronic health records by 30% and seeing a 25% drop in missed appointments after implementing AI appointment scheduling.
Our AI scheduling and triage layer has helped clinics forecast appointment demand by location and specialty, predict no‑show risk, and rebalance slots before bottlenecks formed. In contrast, a triage assistant captured structured symptoms to route patients to the right modality (virtual, urgent, or in‑person), so clinicians saw the right cases at the right time.
This reduced no‑shows, improved schedule utilization without adding staff, shortened time‑to‑appointment, and lifted patient satisfaction through first‑time‑right routing and smoother clinic operations.
Read the full case study to see the impact and workflow details.
KPIs to track: No-show reduction percentage, scheduling latency, call deflection rate, patient satisfaction scores.
Care operations & patient experience agents
In addition to handling preauthorization admin work, smart AI agents now support care teams at every step of the patient journey. From speedy discharge follow-ups to clearer benefits navigation and lightning-fast note-taking, these systems work behind the scenes to close clinical gaps, lift patient satisfaction, and free up clinicians to focus more on actual care.
Discharge & care-plan adherence follow-ups
Twenty percent of Medicare patients are readmitted within 30 days of discharge, often due to inadequate follow-up. Manual post-discharge calls don't scale, and many patients fall through the cracks.
AI agents automate discharge follow-ups by:
- Conducting scheduled check-ins via voice or chat 24-72 hours post-discharge
- Asking structured questions about symptoms, medication adherence, and recovery
- Escalating concerning responses to clinical teams immediately
- Logging patient feedback directly into EHR systems
Healthcare organizations using AI-powered discharge follow-up reduce 30-day readmission rates by 25-35%. Each agent handles 200-300 patient follow-ups daily, saving discharge coordinators 15-20 hours weekly.
Care navigation & benefits guidance
Patients struggle to understand their benefits, find in-network providers, and access the right care at the right time. This leads to unnecessary ER visits, out-of-network bills, and care delays. AI agents provide intelligent care navigation by:
- Explaining benefits in plain language, not insurance jargon
- Suggesting appropriate providers based on specialty, location, and network status
- Routing complex cases to human advocates when needed
- Guiding patients through pre-authorization requirements proactively
Member surveys show 74% want AI plus 24/7 nurse support, and 75% trust AI to book appointments. Additionally, AI navigation reduces administrative call volume by 25% while improving member satisfaction.
Clinical documentation support (human-in-the-loop)
A survey revealed 41% of participating residents reported spending 41-60% of their time not on patient care, but on clinical documentation. Additionally, 37% of participants even said clinical documentation consumed over 60% of their time. This administrative burden drives burnout and reduces medical professionals' clinical capacity.
But what if we tell you that AI agents can save roughly 30-40% of the time spent on these tasks? AI scribe agents support documentation workflows by:
- Transcribing doctor-patient conversations in real-time using ambient listening
- Drafting clinical notes in SOAP or other formats automatically
- Suggesting diagnostic codes and care plan recommendations
- Routing notes to clinicians for review, editing, and signature
Mass General Brigham achieved a 60% reduction in documentation time using AI scribes, giving physicians more face time with patients.
It’s important to note that human scribes still outperform pure AI in complex cases requiring clinical judgment and contextual understanding. So, as a critical safeguard, our AI agents never finalize notes without physician review. Human oversight ensures accuracy and patient safety.
Safety, compliance & governance
Healthcare AI agents must protect patient privacy and meet regulatory standards. Here's how organizations build safe, compliant systems:
- PHI Protection & Encryption
- Encrypt all Protected Health Information (PHI) at rest and in transit using AES-256 encryption
- Use secure vector databases with queryable encryption for AI embeddings
- Implement data redaction and pseudonymization techniques before processing
- Access Controls & Audit Trails
- Deploy role-based access controls (RBAC), limiting who can view PHI
- Maintain immutable audit logs tracking every data access and system action
- Use multi-factor authentication for all system access
- Model Evaluation & Bias Checks
- Test AI models across diverse demographic groups to detect bias
- Set accuracy performance thresholds and flag models that fall below standards
- Conduct regular algorithmic audits using frameworks like STRIDE
- Rollback & Kill-Switch Mechanisms
- Build circuit breaker capabilities to shut down agents exhibiting anomalous behavior immediately
- Implement override mechanisms that don't require agent cooperation
- Run high-autonomy agents in sandboxed environments during early deployment
- Incident Response Plans
- Establish protocols for handling security breaches or data leaks
- Define escalation paths when agents make incorrect clinical recommendations
- Document remediation steps and conduct post-incident reviews
Organizations should sign Business Associate Agreements (BAAs) with AI vendors to ensure HIPAA compliance. At Anglara, we believe that security isn't optional; it's foundational to patient trust and legal protection.

ROI examples
You don’t just have to take our word when we say AI agents deliver solid ROI for healthcare institutions. But we’re sure you’ll believe these real-world organizations reaping benefits:
Prior-authorization automation
Fort HealthCare Ambulatory Surgery Center faced a backlog of weeks' worth of prior authorizations, delaying patient care. After implementing an AI agent for prior-authorization automation, they achieved a 91% success rate in prior-authorization submissions. It saved them 15 minutes per successful submission, so for a practice processing 500 prior authorizations monthly, this translates to:
- Time savings: 500 × 15 minutes = 7,500 minutes (125 hours) monthly
- Staff cost savings: 125 hours × $18.5/hour = $2,312.50 monthly
- Annual savings: $27,750 in staff time alone
Additional benefit: Eliminated weeks of backlog and accelerated patient care delivery
Claim follow-ups automation
A Florida-based internal medicine practice faced billing delays, sharp declines in collections, poor in-house biller performance, and deteriorating accounts receivable. So, they implemented automated medical billing software that processes 1,000 claims per month.
The practice deployed a dedicated team of AR experts, medical billers, and coders to follow up on denied claims and resolve electronic submission issues with Blue Cross Blue Shield (BCBS), thereby eliminating the 2-month paper processing cycles.
Measured outcomes:
- AR days reduced: From 141 days to less than 40 days (72% reduction)
- Patient growth: Base expanded by 400 patients as providers focused more on care
- Cash flow: Regular payment flow established through quality assurance checks on all claims before submission
Patient self-service scheduling
Various organizations are adopting patient self-service scheduling solutions to enhance the patient experience and reduce inbound staff call volume. Patients can view, schedule, cancel, or change appointments, request prescription refills, get directions, or ask questions — all without staff intervention or the need to monitor a chat line.
For example, Main Line Health, a regional health system in Pennsylvania, implemented an AI-powered Call Deflection solution to redirect inbound calls to self-service SMS.
Result: More than 20% of patients calling to schedule mammograms or DEXA scans opted to switch to SMS rather than wait on hold, saving more than 15,000 minutes of call center time.
GPW Health Center, a federally qualified health center in Virginia, did the same and saw 25% of patients choose SMS self-service over waiting on hold, allowing staff to focus on more complex calls.
The business impact:
Digital Call Deflection reduces long wait times, which drive up to 20% of patients to abandon their calls and seek care elsewhere. However, when an organization uses a health system handling 10,000 monthly scheduling calls, they get:
- Calls deflected: 2,000-2,500 calls (20-25%) handled via SMS instead
- Staff time saved: If each call averages 6 minutes, that's 12,000-15,000 minutes (200-250 hours) monthly
- Cost savings: 250 hours × $18.5/hour = $4,625 monthly = $55,500 annually
- Revenue protection: Preventing 20% call abandonment retains patients who would otherwise seek care elsewhere
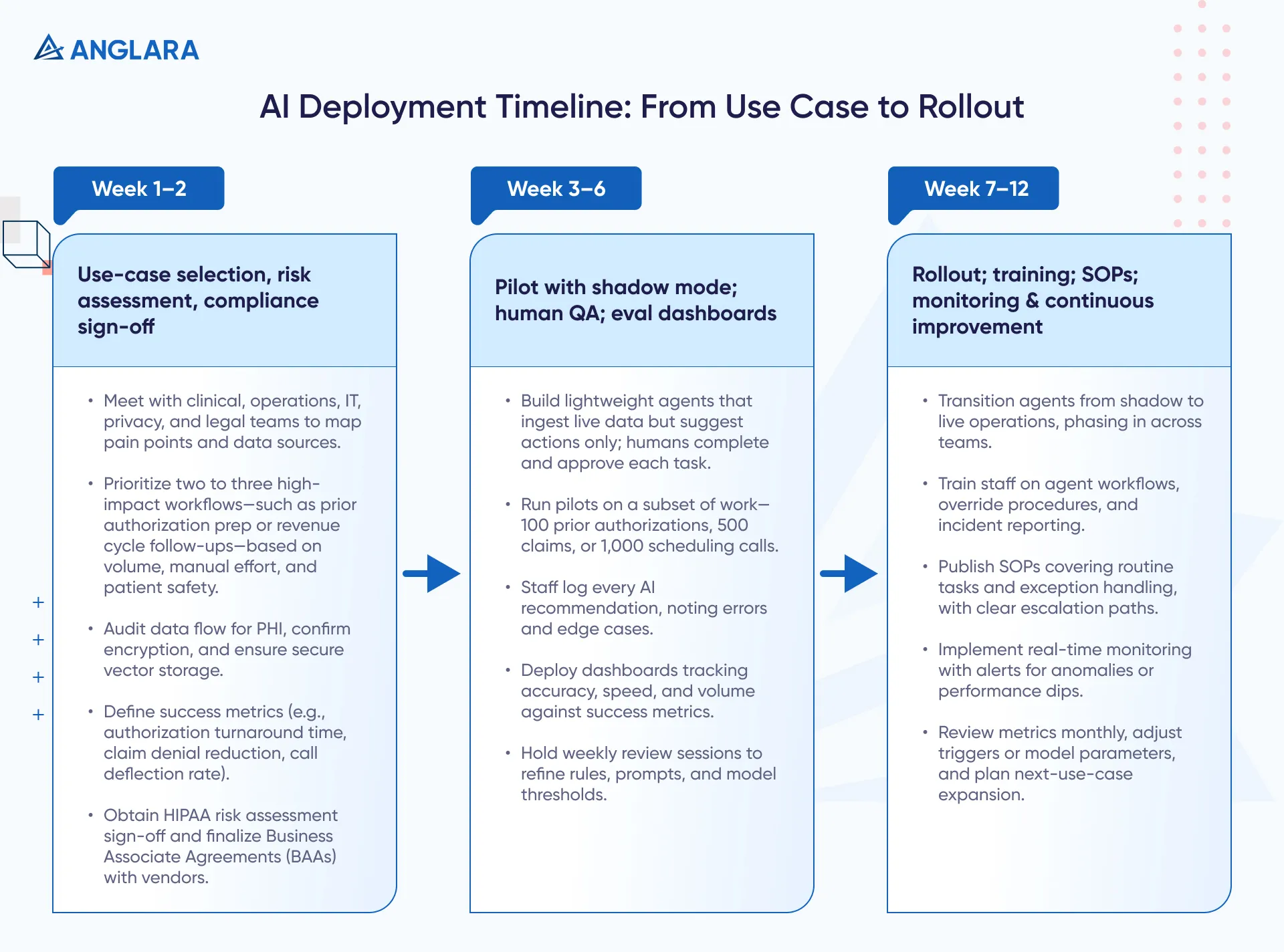
Implementation plan (60–90 Days)
A successful AI agent development and implementation in Healthcare requires a structured approach that carefully considers compliance needs.
Here’s our structured 90-day plan that allows our clients to reduce risks, accelerate time-to-value, and build a strong foundation for scaling AI agents for healthcare successfully:
Conclusion
AI agents are transforming healthcare operations by automating administrative burdens while maintaining patient safety and compliance. Organizations that implement these systems thoughtfully, with proper governance, phased rollouts, and continuous monitoring, can see measurable improvements in staff efficiency, patient satisfaction, and financial performance.
Anglara designs, builds, and deploys HIPAA‑ready AI agents tailored to your workflows. With us, you not only get successful implementation but also end‑to‑end support and staff training for quick ROI. Book a free 30-minute consultation to discuss a HIPAA-ready pilot with us today.
FAQs
Are these agents HIPAA compliant?
Yes, when properly configured. HIPAA-compliant AI agents use end-to-end encryption, secure data storage in U.S. data centers, role-based access controls, and comprehensive audit trails. Organizations must sign Business Associate Agreements (BAAs) with AI vendors and ensure all PHI handling meets the technical, administrative, and physical safeguards required by HIPAA.
Can agents access EHRs safely?
Yes. AI agents integrate with major EHR platforms like Epic and Cerner using secure APIs. They pull necessary data, process it within encrypted environments, and write back structured information without exposing PHI to unauthorized systems. Access is controlled through authentication protocols, and all interactions are logged for compliance audits.
What tasks must stay with clinicians?
Use human-in-the-loop workflows in which AI drafts content while clinicians retain final authority over patient care. Tasks requiring clinical judgment, empathy, or complex case interpretation should always involve human oversight.
How do we audit decisions?
AI agents generate immutable audit trails, logging every action, data access, and recommendation. Healthcare organizations can review these logs to verify compliance, investigate errors, and demonstrate regulatory adherence. Our dashboards provide real-time visibility into agent performance, including accuracy rates, processing times, and flagged anomalies.
What are typical costs and timelines?
Costs and timelines depend on your use case, data readiness, EHR integration, compliance scope, and the level of human oversight you want. Workflow complexity, volumes, and change management also shape build effort and ongoing spend. Fixed-fee pilots or usage-based models both work when KPIs and guardrails are clear. Anglara can design a HIPAA-compliant plan tailored to your budget and goals. Book a free consultation today to get a tailored.





